In February 2015, Sidney Kennedy gave a presentation on the topic ‘Neurocognition and Function – The Next Frontier in Treating Major Depressive Disorder?’ Kennedy, Professor of Psychiatry at St Michael’s Hospital and University of Toronto, Canada, has treated depression for over three decades and over this period has observed a shift in treatment goals. This article highlights key points from his presentation.
Objectives
- Identify specific cognitive difficulties in MDD patients
- Consider symptoms + cognition + function in your assessment and management plans
Change Thinking to Improve Thinking
There has been a shift from the treatment goal of symptom reduction to achieving functional remission. The aim is for a patient to resume a high quality life. When asked about the outcomes they most value, patients with depression give priority to positive mental health – which includes optimism, vigour and self-confidence, feeling like their usual selves, and a return to normal levels of functioning at home and work. According to the survey by Zimmerman et al.1, these features – from the patient’s perspective – rank above reduction in symptoms of depression per se.
Cognition is central to the positive mental health and functioning treasured by patients, and it is an aspect of depression that we have neglected. In treating depression, we generally do a reasonably good job: by classical criteria based on symptom reduction, the response rate to first line treatment is around 50%. But we can always do better. Homogeneous treatments are being used to tackle a heterogeneous disorder, and there are currently no objective biological measures on which to base diagnosis, prognosis or treatment selection.
One way to improve patient outcomes is to hold cognition in mind – as well as core depressive symptoms – when assessing patients, designing management plans and evaluating response.
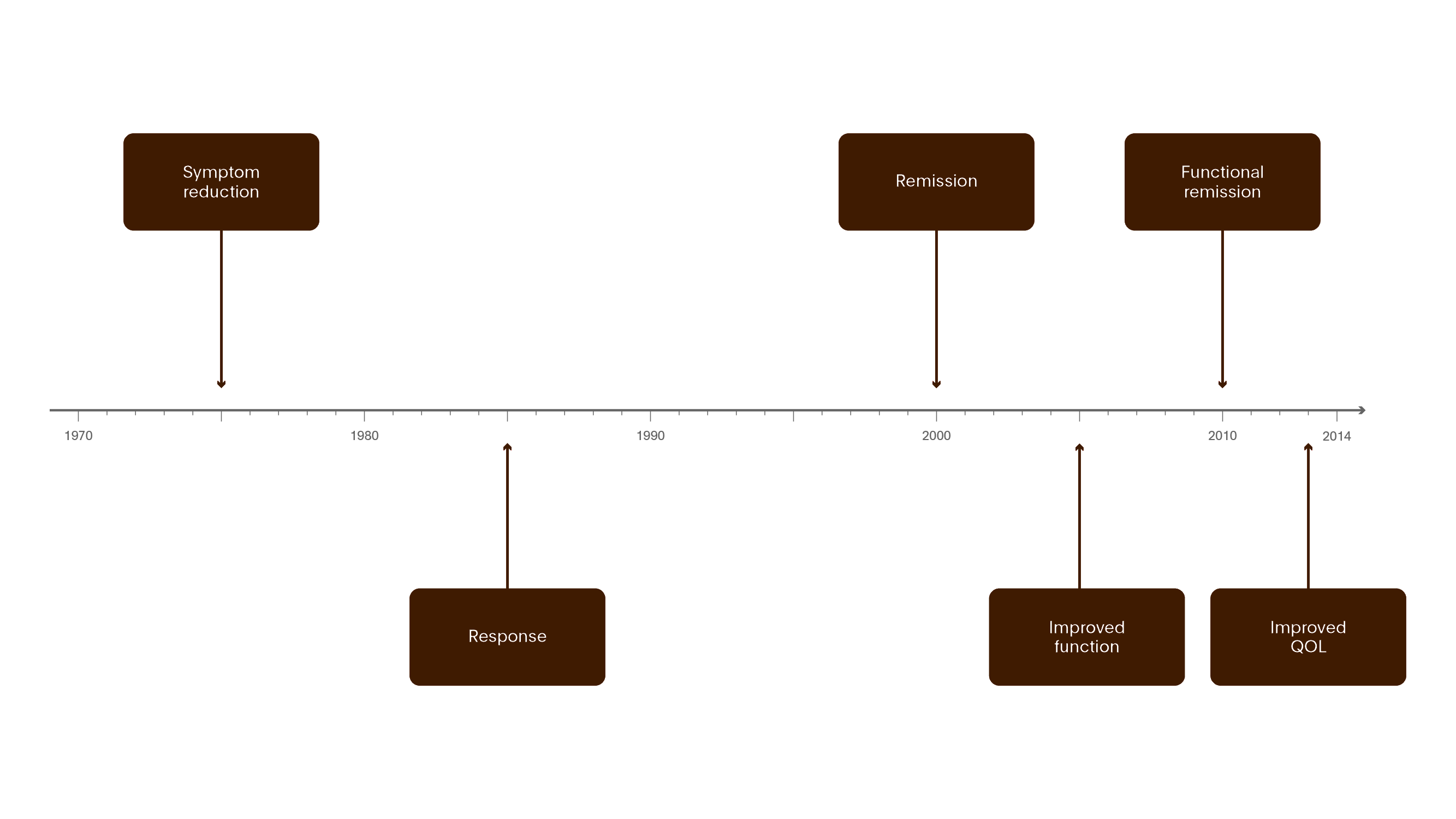
Figure 1. Evolving goals for MDD Treatment
The past two decades have seen the aims of treatment broaden from a focus on the relief of depression symptoms to include functional and cognitive and quality of life.12
QOL = quality of life

Figure 2. What patients want
When asked about outcomes they value, patients with depression cite positive mental health and a return to normal feelings and functioning – at home and work. Absence of the symptoms of depression in themselves was given a lower priority.1
- Response rate to first line treatment is 50%
- Many patients are treatment resistant
- There are no objective biological measures on which to base diagnosis, prognosis, or treatment selection
Hold Cognition in Mind
For years, we have focused on depression as a mood disorder, and on features such as anhedonia. We have tended to believe that any cognitive deficits are secondary to the depression, and that they will go away once the depressed mood lifts. In addition, at a practical level, cognitive problems have been seen as difficult to assess, since neuropsychological testing is regarded as time consuming. We can now challenge all of these views.
Why has cognition in depression been ignored in the past?
- Belief that cognitive dysfunction is not a core feature of depression
- Schizophrenia and dementia are disorders of cognition – depression and bipolar disorder are mood disorders
- Neuropsychology testing takes so long and how is it relevant?
- Can it be treated?
- Doesn’t “pseudodementia” remit?
Why Cognition in Depression Should Be Explored, Not Ignored
- Recognition of employment and health costs tied to depression
- Neurocognition is directly associated with functional outcomes
- Cognitive deficits
- may predate onset of major depression
- contribute to impairment during the depressive episode
- predict poorer functional outcomes even after symptom response and remission
- Depression-associated “pseudodementia” does not simply go away when mood improve
- Costs of depression include cognitive impairment
Advances in neuroimaging are revealing the detailed neurocircuitry involved
- Antidepressants differ in their impact on cognition
- New non-pharmacological treatments may improve cognitive outcomes, and therefore, functional outcomes
A recent review by Rock et al.2 posed the question of whether cognitive impairment should be considered a core feature of depression that may be a valuable target for treatment. It was concluded that both low mood and cognitive impairment are associated with poor psychosocial functioning, and that cognitive impairment represents a core feature of depression that should not be considered secondary to symptoms of low mood.
Cognitive deficits and resulting loss of function are a big deal – to an individual and to society as a whole. Significant employment and health costs are tied to depression. The impact on work performance is highlighted in an observational study by Koopmans et al.3 Between 2002 and 2005, they evaluated 15% of the Dutch working population and identified 9,910 new absence episodes due to depression. The mean duration of sickness absence due to depressive symptoms was 200 and 213 days in men and women, respectively. Older employees had longer absence durations. The rate of chronicity (1 year of absence) was 24%.
Evidence for Cognitive Deficits in Depression
There is accumulating evidence on the nature and extent of cognitive impairment in depression, and of its correlates in neuro-anatomy and function.
Depressive symptoms may be associated with increased risk of developing dementia.4 In a 5-7 year follow-up of depressed individuals, the relative risk for developing dementia was 3.93.5
Depression is associated with several cognitive deficits including working memory, executive function, episodic memory and processing speed.6 A study of more than eight thousand outpatients suggests that capacity for delayed recall declines steadily with the number of previous depressive episodes.7
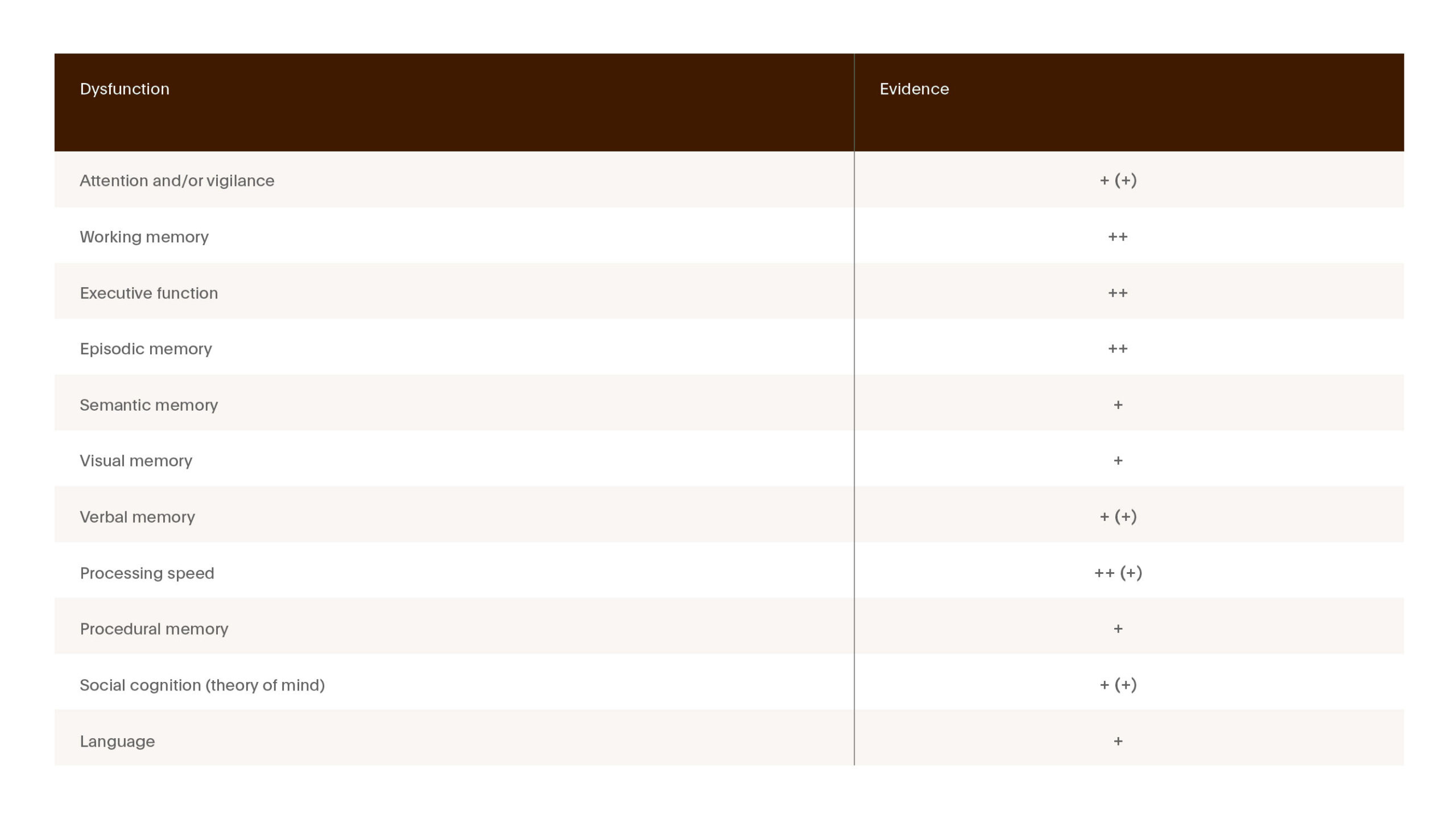
Figure 3. Evidence for neuropsychological dysfunction in depression
There is evidence for neuropsychological dysfunction spanning many cognitive domains. Well documented for: memory, processing speed, executive function. Effects on social cognition may also be important. Depressed patients have altered perception of emotional cues as facial expression and body movement.6
- 0 – Essentially absent
- 0/+ – Poorly documented, ambiguous, mild and/or variable
- + – Consistently present but not pronounced
- ++ – A common marked characteristic
- ? – Not clearly evaluated
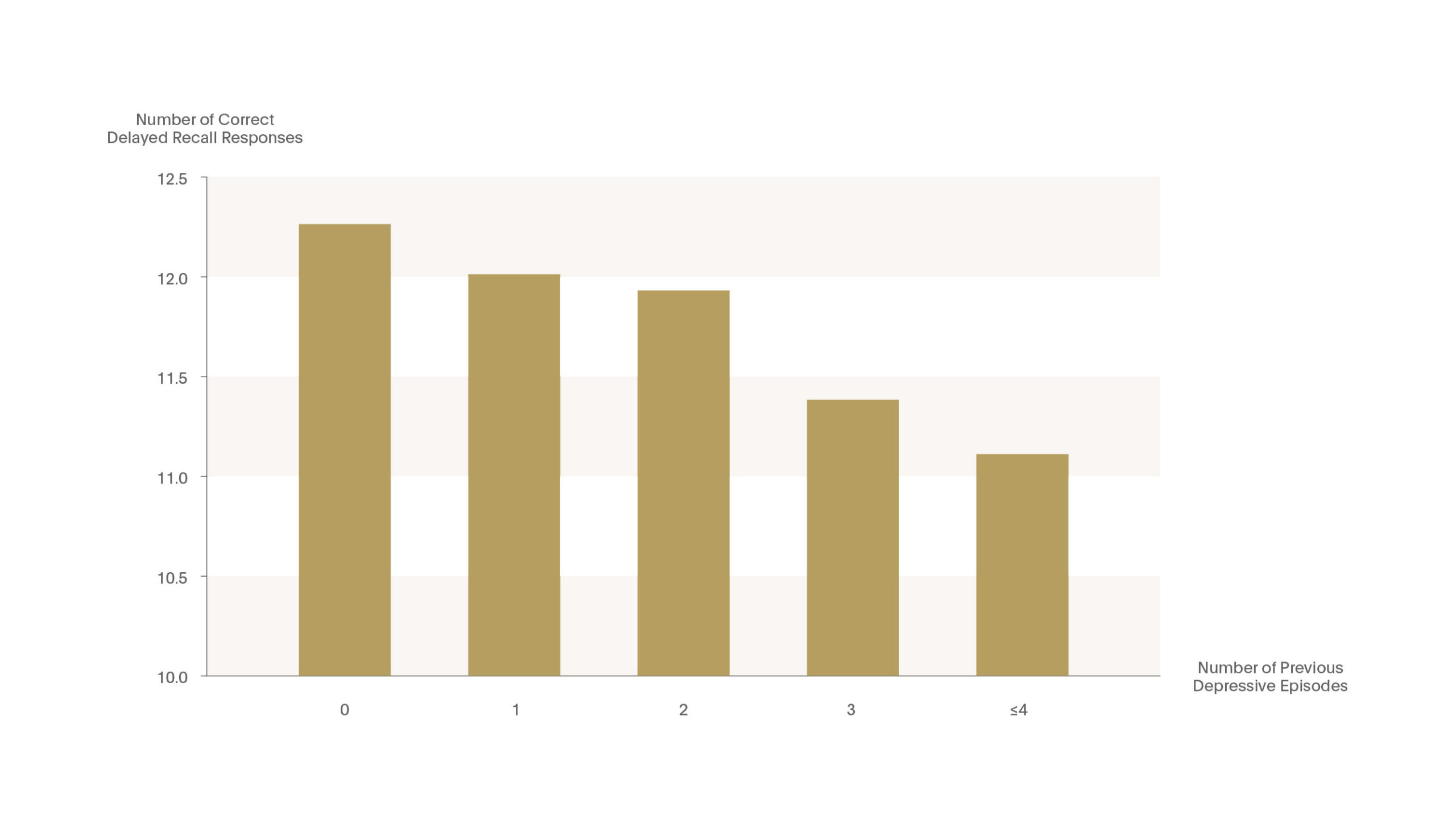
Figure 4. Memory function declines with increasing number of major depressive episodes
A study in outpatients with MDD (n=8229) suggests the capacity for delayed recall declines steadily with the number of previous depressive episodes. Among 1800 depressed patients in remission who had responded within 6 weeks, the number of recalled words was related to the number of previous episodes. Delayed recall capacities fell by 2-3% for each prior episode.7
Heritability of Cognitive Deficits in MDD
Investigators have also worked with data from Danish twin registries.8
- Danish twin registry linked to Psychiatric Central Research Register
- 94 identical and fraternal high risk vs. 88 low risk twins
- Completed Trials A+B and Stroop
- Psychologically healthy members of a twin pair in which the other member had depression showed lower performance on several measures of cognitive function.
- In the case of executive function, the effect in monozygotic pairs was greater than that in dizygotic pairs.
- Results suggest the heritability of cognitive deficits in MDD, and support the hypothesis that cognitive impairment is present before the onset of the affective disorder.
Cortical Thining and Neurocognitive Deficits in MDD
A three-generation cohort study of 131 participants who had either high- or low-familial risk for developing MDD and had structural MRI,9 identified a brain-based endophenotype for MDD that includes cortical thinning on lateral right hemisphere and medial left hemisphere in MDD and high risk groups. The magnitude of cortical thinning correlates with inattention and poor visual memory for social stimuli.
Abnormal Hippocampal Activation in MDD
Abnormal hippocampal activation has also been observed in MDD.10 Milne and colleagues compared patients who experienced 3 or more previously treated depressive episodes (n=22) with age- and sex-matched controls (n=18). Functional MRI data were collected while participants performed a recollection memory process dissociation task. Activation of the right hippocampal and left parahippocampal gyrus was increased in controls compared with patients with MDD, suggesting that the brain of depressed patients has to ‘work harder’ to achieve the same result.
Improved Mood and Improved Cognition Don’t Go Hand in Hand
Crucially, we should no longer accept the view that cognitive impairments will invariably disappear with successful treatment. Rock et al assessed whether cognitive is a core feature of depression that may be a treatment target.2 The meta-analysis used the Cambridge Neuropsychological Test Automated Battery (CANTAB) to assess cognitive function in patients with depression during symptomatic and remitted states.
- All Subjects (700 MDD, 700 healthy controls)
Executive function, memory and attention - Un-Medicated (270 MDD, 270 healthy controls)
Executive function and attention - Remitted MDD (170 MDD, 170 healthy controls)
Significant deficits in executive function and attention
Cognitive deficits in executive function, memory and attention were observed in MDD relative to controls. In addition, moderate deficits in executive function, attention and memory persisted in remitted patients. This indicates that cognitive impairment occurs separately from low mood. Compared with 170 healthy controls, significant deficits in executive function and attention remained, despite the resolution of mood symptoms. Cognitive problems do not necessarily resolve in synchrony with other core elements of depression. The authors conclude that cognitive impairment cannot be considered entirely secondary to symptoms of low mood, and that it may be a valuable target for future interventions.
Identifying a problem is the first step towards managing it. It is indeed true that neuropsychological testing used to be time-consuming, but new cognitive test batteries can now be completed in 10‑15 minutes, and some can be self-administered.
Measuring Cognitive Deficits
In terms of treatment, Christopher Bowie and colleagues are showing benefits using a computerised system that engages patients in game-type tasks lasting ninety minutes that relate to areas of cognitive function previously identified as requiring attention.11

Figure 5. Measuring cognitive deficits
Cognitive deficits can be assessed by patient self-report. But given the nature of depression, including the tendency to negative bias, these may not be as useful as objective neuropsychological tests.
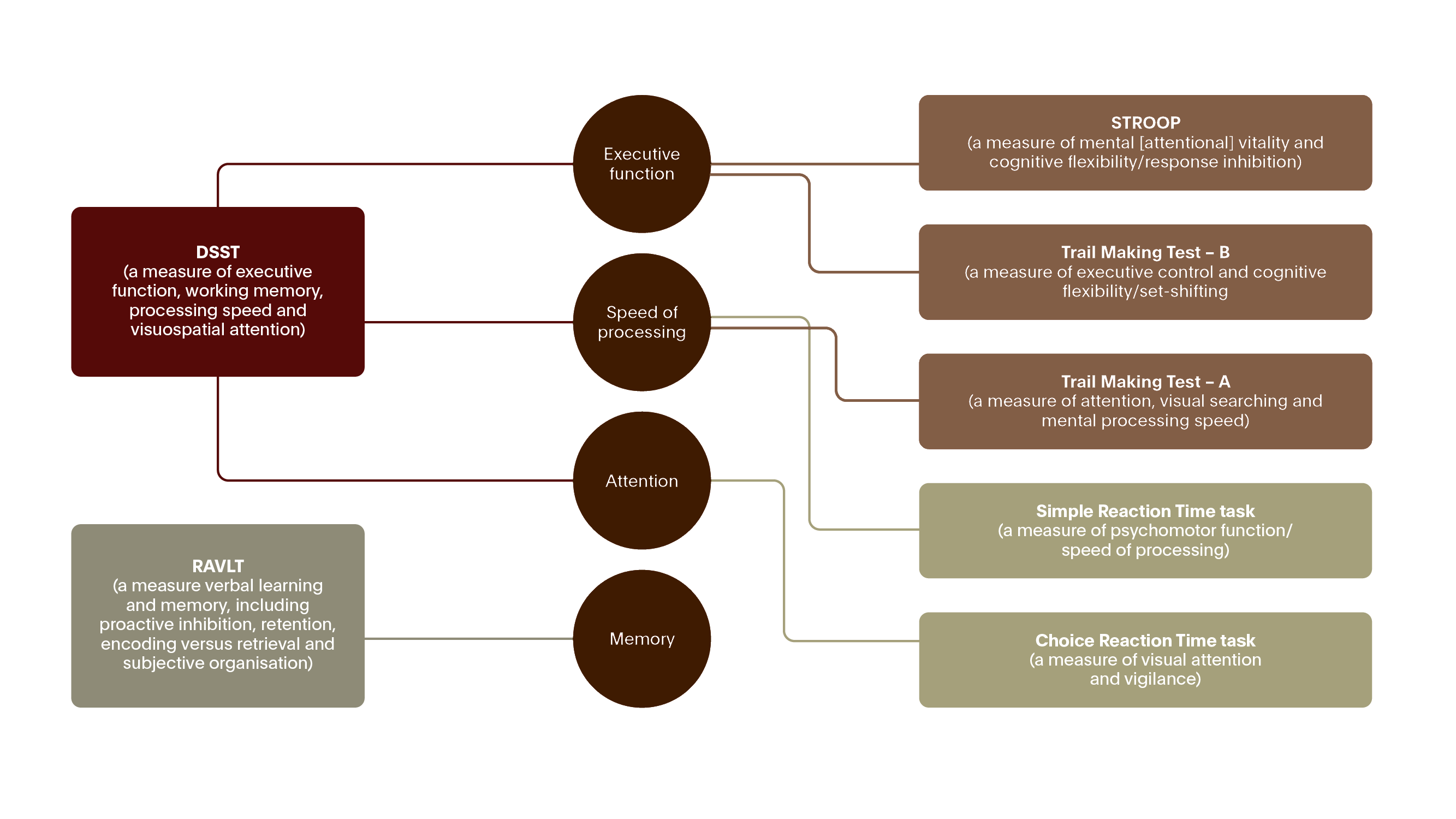
Figure 6. Neuropsychological tests to measure performance on cognitive domains affected in MDD12
DSST = Digit Symbol Substitution Test
RAVLT = Rey Auditory Verbal Learning Test
Targeting Cognitive Deficits in MDD
Our choice of antidepressant can also have a positive or a negative impact on cognitive symptoms in depression, depending on their mechanism of action.
Targeting cognitive deficits in MDD – Cognitive remediation:
- Potential aim to exercise specific pathways with the goal of remediating specific areas of cognitive function
- Methods: Using behavioural strategies to improve a range of neuropsychological domains such as memory and executive functioning
- Techniques: Cognitive control training sessions, computer games, group discussion, homework, application to real life situations
Examples of Tests Relevant to Cognitive Domains Affected by MDD
- Digit Symbol Substitution Test: executive function, speed of processing and attention
- Rey Auditory Verbal Learning Test: learning and memory
- British Columbia Cognitive Complaints Inventory: memory, concentration, thinking speed, problem solving